|
About one of every three adult Americans currently
have hypertension, yet a surprising number don’t
know they have it and less than half have their high
blood pressure under control—leading many health
experts to refer to the condition as a “silent
killer”.
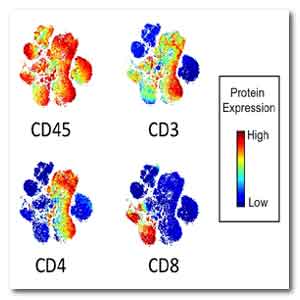
IMAGE: Four types of immune T cells from an adult
with normal blood pressure cluster on a CyTOF map.
Source: Meena Madhur, Vanderbilt University School
of Medicine, Nashville
For many folks, blood pressure control can be
achieved through lifestyle changes, such as losing
weight, exercising, limiting salt intake, and taking
blood pressure medicines prescribed by their
health-care provider.
Unfortunately, such measures don’t work for
everyone, and some people continue to suffer damage
to their kidneys and blood vessels from poorly
controlled hypertension.
Meena Madhur, a physician-researcher at Vanderbilt
University School of Medicine, Nashville, wants to
know whether the immune system might be playing a
role, and whether this might hold some clues for
developing new, more targeted ways of treating high
blood pressure.
To get such answers, this practicing cardiologist
will use her 2016 NIH Director’s New Innovator Award
to conduct sophisticated, single-cell analyses of
the immune systems of people with and without
hypertension.
Her goal is to produce the most comprehensive
catalog to date of which human immune cells might be
involved in hypertension.
Back in the 1960s, animal studies provided the first
indication that the immune system might play a role
in hypertension.
But with a relatively limited set of tools available
then to explore the immune system, limited progress
was made over the ensuing few decades.
Then, thanks to advances in knowledge and technology
arising from the genomic revolution, that line of
inquiry began to move forward about a decade ago,
starting with more sophisticated studies on the role
of immunity and inflammation in hypertension,
focusing on genetically engineered rodents.
Now, Madhur is taking the next step with a research
project focused on humans.
To date, she and her colleagues have collected blood
samples from a pilot group of 39 adult volunteers—23
with hypertension and 16 without.
These groups are carefully matched for age and body
mass index (BMI), two strong risk factors for
hypertension.
To get the data, her group will work with Vanderbilt
colleague Jonathan Irish, an expert in Cytometry by
Time-of-Flight (CyTOF) technology, who will assist
in panel design, validation, and data analysis.
CyTOF is a form of mass cytometry in which
individual antibodies are labeled in the lab with
heavy metal tags for visualization, instead of the
customary fluorescent tags.
This gives Madhur more channels to work with than
fluorescence flow cytometry, allowing her team to
pack a lot more antibody markers onto each cell,
thus increasing the chances of finding something
interesting.
CyTOF has been used in cancer studies and to monitor
a type of immune T cell that is affected by the
human immunodeficiency virus, the cause of AIDS.
In the Accelerating Medicines Project (AMP), it’s
also being used to look at immune cells in biopsies
from patients with rheumatoid arthritis and lupus.
But CyTOF has never been applied on such a
comprehensive scale to monitor the immune system in
hypertension.
Irish has developed a computer software program that
employs machine learning to map similarities in the
antibody markers attached to the millions of immune
cells processed from the blood samples.
Each dot plotted on the map represents an individual
cell, and the dots cluster into distinct islands of
T cell subsets, B cell subsets, and innate immune
cells.
The more distance between each dot, the more
dissimilar their molecular characteristics are.
According to Madhur, flow cytometry allows you to
find what you are looking for, while CyTOF allows
you to find what you never knew existed.
Madhur will look for any unique clusters of cells on
the map that come only from people with
hypertension.
If so, she will pick out eight to 12 features from
those cells that will allow isolation by traditional
flow sorting and then further characterize these
cells in vitro.
She will also follow up on her initial leads by
opening her study to more volunteers with a wider
range of BMIs and age to determine if hypertension
associated changes in the immune system track with
aging and obesity.
For more information
U.S. National Institutes of Health
Link...
MDN |