|
Pathologists often disagree on diagnoses of "gray
zone" moles. Diagnoses within the disease spectrum
from moderately dysplastic nevi to early stage
invasive melanoma are neither reproducible nor
accurate.
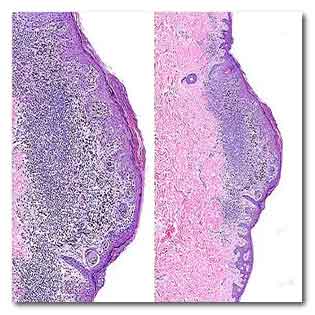
With this tissue sample, the interpretations of
36 pathologists ranged from “common nevus,” the
technical term for a benign mole, to invasive
melanoma. The consensus reference panel judged it to
be a Class III melanoma in situ.
UW Medicine.
Every year, millions of Americans have a suspicious
mole or skin lesion biopsied and sent to a
pathologist to learn whether it is a potentially
deadly melanoma.
The pathologist’s interpretation is important: if
the lesion is judged to be benign, no treatment may
be recommended, but if malignant, the patient will
typically undergo surgery and possibly other
treatments.
New research indicates that pathologists are likely
to agree when lesions are benign or highly
malignant, but often disagree when gray-area lesions
are less obviously characterized.
What’s more, the pathologists in the study not only
often disagreed with the interpretations of a
consensus reference panel of experts, they also
often disagreed with their own interpretations when
shown the same biopsy samples eight or more months
later.
The study appears June 28 2017 in The BMJ (British
Medical Journal). Its lead author was Dr. Joann G.
Elmore, a professor of medicine at the University of
Washington School of Medicine in Seattle.
“We found that pathologists’ interpretations of
biopsies for certain gray-area lesions indicate that
accuracy and reproducability can be affected,”
Elmore said. “These findings underscore how
challenging it may be to make these judgements in
clinical practice.
Such interpretations could be improved by using a
standardized classification system, which could
reduce the risk of misdiagnosis and inappropriate
treatment.”
The investigation involved 187 experienced
pathologists in 10 states, who had volunteered to
participate.
In the study’s first phase, each was asked to review
and interpret 48 cases randomly selected from 240
skin biopsies.
In the second phase, 118 of the pathologists viewed
the same set of slides that they had interpreted
before but shuffled in a different order.
At least eight months had passed between the first
and second viewings of the slides.
The pathologists’ interpretations were then
organized with the Melanocytic Pathology Assessment
Tool and Hierarchy for Diagnosis (MPATH-Dx)
histology form, which placed each interpretation
into one of five diagnostic classes:
I) benign lesions that require no further treatment;
II) moderately abnormal lesions in which the removal
of a small margin of tissue around the lesion is
suggested;
III) severely abnormal lesions, including melanoma
in situ, in which a slightly larger margin is
suggested;
IV) early stage invasive melanoma, in which case a
margin =1 cm is recommended;
(V) higher stage invasive melanoma, in which case a
wide excision, =1cm, is recommended with possible
additional treatment, including sentinel lymph node
biopsy and adjuvant radiation or chemotherapy.
The researchers found that the participating
pathologists agreed with the consensus panel’s
interpretation in 92 percent of the benign Class I
cases and in 72 percent of the Class V higher-stage
invasive melanomas.
However, participants agreed with the panel’s
consensus diagnosis in 25 percent of the Class II
cases, 40 percent of the Class III cases and 43
percent of the Class IV cases.
“This low level of diagnostic precision is of
clinical concern,” the researchers wrote. “Although
diagnostic discordance has been described in other
areas of clinical medicine, including pathologists
diagnosing breast biopsies and radiologists
interpreting mammograms, the findings reported here
are more pronounced than in other fields of
medicine.”
Dr. Michael Piepkorn, a UW clinical professor of
dermatology and senior author of the study, offered
this context:
"The findings reflect the emerging realization that
a large gray zone of intermediate moles exists
between common moles and fully developed melanoma.
The diagnostic processes developed over past
generations of pathologists do not reliably
discriminate between the intermediate moles that are
clinically harmless versus those that harbor changes
that will worsen over time and ultimately become
malignant.”
In an associated opinion piece also in The BMJ,
Elmore emphasized that "the diagnostic variability
that we found does not mean that pathologists are
the problem.” She added that "pathologists embrace
this responsibility with the utmost skill and
thoughtful commitment.”
In addition to adopting more standardized
classification systems, physicians could communicate
to patients that there are limits to medical
professionals’ ability to classify skin lesions, the
researchers wrote.
“We propose adding standardized statements to
pathology reports reminding readers that melanocytic
lesions are challenging to interpret and that
variability exists among pathologists, especially in
the middle diagnostic classes,” they wrote.
Invasive melanoma kills more than 9,000 Americans a
year.
For more information
The BMJ (British Medical Journal)
Pathologists’ diagnosis of invasive melanoma and
melanocytic proliferations: observer accuracy and
reproducibility study
Link...
MDN |