News and Insights for
your best life. Online since 1998
- Home Health
- Breaking news
- In caso di...
- Per saperne di
più... - Medicina occidentale
- Medicine complementari
- Medicina cinese
e agopuntura - Omeopatia
- Fitoterapia

Scientists designed a way to target and destroy specific DNA sequences in microbes, thus removing harmful bacterial genes. The approach might be used to develop therapies against pathogenic bacteria, including those resistant to multiple antibiotics.
Over time, many bacteria have adapted to the drugs designed to kill them, making antibiotics less effective. Diseases such as tuberculosis, gonorrhea, and a variety of healthcare-associated infections are now difficult to treat when they’re caused by multidrug-resistant bacteria. New approaches are needed to address this growing problem.
Antibiotics work by disrupting bacteria’s ability to grow and replicate. These drugs tend to be broad spectrum, affecting both beneficial and harmful bacteria. Dr. Timothy K. Lu at the Massachusetts Institute of Technology, with graduate students Robert Citorik and Mark Mimee, set out to develop a way to specifically target harmful bacteria.
Bacteria have evolved systems to protect themselves against invaders. One of these, the CRISPR-Cas immune system, features clusters of short, repeated DNA sequences separated by other short stretches called spacers.
These spacer sequences are created from the genetic material of bacteriophages (viruses that attack bacteria) and plasmids (pieces of DNA exchanged between bacteria) that the cell or an ancestor encountered. The spacers provide immunity to future exposure by directing enzymes called nucleases—encoded by cas (CRISPR-associated) genes—to destroy those specific genetic sequences.
The researchers reasoned that they could modify the spacers to target specific genetic sequences associated with bacterial virulence or antibiotic resistance. The work was funded in part by an NIH Director’s New Innovator Award and NIH’s National Institute of General Medical Sciences (NIGMS). Results appeared online on September 21, 2014, in Nature Biotechnology.
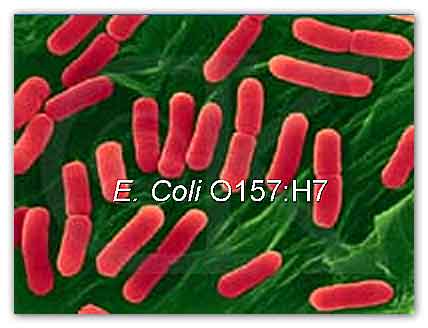
The team used a CRISPR-Cas system to successfully target antibiotic resistance genes in E. coli. Components of the system could be delivered either by bacteriophages or by other bacteria via conjugation (a process by which bacteria exchange genetic material). Both effectively spread through E. coli populations. The system could target genes on bacterial chromosomes or plasmids.
The team also tested whether they could target a known virulence factor that allows the pathogen E. coli O157:H7 to colonize intestines. Using bacteriophage to deliver a CRISPR-Cas system against the gene, they saw a 20-fold reduction in viable E. coli cells. The team tested this system in greater wax moth larvae, an infection model often used to predict virulence in mammals. The system significantly improved survival in larvae infected with E. coli O157:H7.
The researchers were able to target multiple resistance genes at once by including 2 spacers with DNA from 2 different antibiotic resistance genes. In addition, the system could discriminate between targets that differed by only a single nucleotide. Finally, the team showed that the system could be used to selectively kill a specific E. coli strain in a population based on its genetic content while leaving others untouched.
“This is a pretty crucial moment when there are fewer and fewer new antibiotics available, but more and more antibiotic resistance evolving,” Lu says. “We've been interested in finding new ways to combat antibiotic resistance.” The researchers are now working to further improve delivery of the CRISPR-Cas system components.
For more information
Sequence-specific antimicrobials using efficiently delivered RNA-guided nucleases
the Massachusetts Institute of Technology MIT
U.S. National Institutes of Health (NIH)
MDN
del Dott. Turetta
Quali sono i problemi o le disfunzioni che possono giovarsi di un intervento omeopatico d'urgenza e, di conseguenza, come dovrebbe essere un ideale armadietto medicinale omeopatico casalingo.- Home -
- Health -
- Depressione -
- Sexuality
- Environment -
- Food -
- Musica -
- Capirsi -
- Grafologia -
- Ridere
Copyright © 1998/2018 www.mybestlife.com tutti i diritti sono riservati eccetto quelli già di altri proprietari.
.In caso di
Pubblicità
Per saperne di più su
Pubblicità
Pubblicità
Pubblicità
Pubblicità


