|
Emulsifiers, which are added to most processed foods
to aid texture and extend shelf life, can alter the
gut microbiota composition and localization to
induce intestinal inflammation that promotes the
development of inflammatory bowel disease and
metabolic syndrome, new research shows.
The research, published Feb. 25 in Nature, was led
by Georgia State University Institute for Biomedical
Sciences’ researchers Drs. Benoit Chassaing and
Andrew T. Gewirtz, and included contributions from
Emory University, Cornell University and Bar-Ilan
University in Israel.
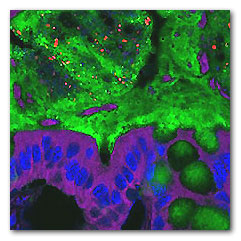
Mice fed emulsifiers had bacteria (red) deep in the
mucus layer (green) so they were closer to
intestinal cells (purple and blue) than they should
be. Image by the researchers.
Inflammatory bowel disease (IBD), which includes
Crohn’s disease and ulcerative colitis, afflicts
millions of people and is often severe and
debilitating. Metabolic syndrome is a group of very
common obesity-related disorders that can lead to
type-2 diabetes, cardiovascular and/or liver
diseases.
Incidence of IBD and metabolic syndrome has been
markedly increasing since the mid-20th century.
The term “gut microbiota” refers to the diverse
population of 100 trillion bacteria that inhabit the
intestinal tract. Gut microbiota are disturbed in
IBD and metabolic syndrome. Chassaing and Gewirtz’s
findings suggest emulsifiers might be partially
responsible for this disturbance and the increased
incidence of these diseases.
“A key feature of these modern plagues is alteration
of the gut microbiota in a manner that promotes
inflammation,” says Gewirtz.
“The dramatic increase in these diseases has
occurred despite consistent human genetics,
suggesting a pivotal role for an environmental
factor,” says Chassaing. “Food interacts intimately
with the microbiota so we considered what modern
additions to the food supply might possibly make gut
bacteria more pro-inflammatory.”
Addition of emulsifiers to food seemed to fit the
time frame and had been shown to promote bacterial
translocation across epithelial cells. Researchers
hypothesized that emulsifiers might affect the gut
microbiota to promote these inflammatory diseases
and designed experiments in mice to test this
possibility.
Dietary emulsifiers are added to many processed
foods to improve texture and extend shelf life.
Chemically similar to detergents, they have been
shown to alter the mucus barrier and the microbes
associated with it.
To determine whether these might play a role in
chronic diseases, the team fed mice low levels of 2
commonly used emulsifiers, carboxymethylcellulose or
polysorbate-80, in drinking water or in food at
doses seeking to model the broad consumption of the
numerous emulsifiers that are incorporated into
almost all processed foods. They observed that
emulsifier consumption changed the species
composition of the gut microbiota and did so in a
manner that made it more pro-inflammatory.
The altered microbiota had enhanced capacity to
digest and infiltrate the dense mucus layer that
lines the intestine, which is normally, largely
devoid of bacteria. Alterations in bacterial species
resulted in bacteria expressing more flagellin and
lipopolysaccharide, which can activate
pro-inflammatory gene expression by the immune
system.
Mice fed the emulsifiers for 12 weeks developed
low-grade intestinal inflammation and metabolic
syndrome characterized by increased levels of food
consumption, obesity, hyperglycemia and insulin
resistance, a group of conditions that increase the
risk for type 2 diabetes, heart disease, and stroke.
Mice that were genetically engineered to be more
prone to inflammation and gut microbe changes
developed colitis when fed the emulsifiers.
Mice that consumed the emulsifiers had an altered
bacterial composition and thinner intestinal mucus,
so that bacteria were closer to the cells lining the
colon. The mice also had weight gain, increased food
consumption, increased fat mass, and impaired
glucose handling, a sign of metabolic syndrome.
When the team fed emulsifiers to germ-free mice,
which don’t have gut microbiota, the mice showed no
signs of gut inflammation, mucus thinning, or
metabolic syndrome.
This suggests that the effects of the emulsifiers
were most likely caused by altering gut bacteria.
When gut microbes from normal, emulsifier-fed mice
were transplanted into germ-free mice that hadn’t
been fed emulsifiers, the mice developed low grade
inflammation, increased fat mass, and glucose
intolerance. These results showed that changes in
the gut microbiota caused by dietary emulsifiers can
drive inflammation and metabolic changes.
“We do not disagree with the commonly held
assumption that over-eating is a central cause of
obesity and metabolic syndrome,” Gewirtz says. But
these results suggest that modern additions to the
food supply can interact with gut microbiota to
influence inflammation, metabolism, and weight.
The group is now testing additional emulsifiers.
They are also designing experiments to examine the
effects of food additives in humans.
The research was funded in part by NIH’s National
Institute of Diabetes and Digestive and Kidney
Diseases (NIDDK). Findings appeared in Nature on
March 5, 2015.
For more information
Dietary emulsifiers impact the mouse gut microbiota
promoting colitis and metabolic syndrome.
Chassaing B, Koren O, Goodrich JK, Poole AC,
Srinivasan S, Ley RE, Gewirtz AT. Nature. 2015 Mar
5;519(7541):92-6. doi: 10.1038/nature14232. Epub
2015 Feb 25. PMID: 25731162.
Georgia State University
US
National Institutes of Health (NIH)
MDN |