|
The most frequent indication for knee arthroscopy is
degenerative joint disease in middle aged and older
patients. Each year, more than 700.000 knee
arthroscopies are done in the United States and
150.000 in the United Kingdom.
Magnetic resonance imaging evidence of meniscal
abnormality, osteophytes, cartilage damage, and bone
marrow lesions is often present.
All these imaging abnormalities are common in the
general population and are often asymptomatic.
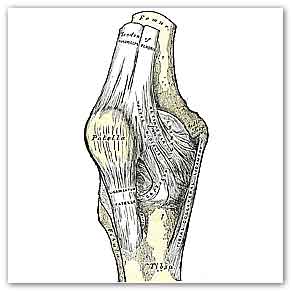
Knee joint
The evidence base for arthroscopic surgery is known
to be weak, and a pressing need exists for more high
quality multicentre randomised controlled trials,
systematic reviews, and meta-analyses to inform
clinicians and improve care for patients.
Researchers have already reported that trials of
arthroscopic surgery find no benefit over control
interventions ranging from exercises to placebo
surgery.
To determine benefits and harms of arthroscopic knee
surgery involving partial meniscectomy, debridement,
or both for middle aged or older patients with knee
pain and degenerative knee disease systematic
searches for benefits and harms were carried out in
Medline, Embase, CINAHL, Web of Science, and the
Cochrane Central Register of Controlled Trials
(CENTRAL) up to August 2014. Only studies published
in 2000 or later were included for harms.
Randomised controlled trials assessing benefit of
arthroscopic surgery involving partial meniscectomy,
debridement, or both for patients with or without
radiographic signs of osteoarthritis were included.
For harms, cohort studies, register based studies,
and case series were also allowed.
The search identified nine trials assessing the
benefits of knee arthroscopic surgery in middle aged
and older patients with knee pain and degenerative
knee disease.
The main analysis, combining the primary endpoints
of the individual trials from three to 24 months
postoperatively, showed a small difference in favour
of interventions including arthroscopic surgery
compared with control treatments for pain (effect
size 0.14, 95% confidence interval 0.03 to 0.26).
This difference corresponds to a benefit of 2.4 (95%
confidence interval 0.4 to 4.3) mm on a 0-100 mm
visual analogue scale.
When analysed over time of follow-up, interventions
including arthroscopy showed a small benefit of 3-5
mm for pain at three and six months but not later up
to 24 months.
No significant benefit on physical function was
found (effect size 0.09, −0.05 to 0.24).
Nine studies reporting on harms were identified.
Harms included symptomatic deep venous thrombosis
(4.13 events per 1000 procedures), pulmonary
embolism, infection, and death.
The small inconsequential benefit seen from
interventions that include arthroscopy for the
degenerative knee is limited in time and absent at
one to two years after surgery.
Knee arthroscopy is associated with harms.
Taken together, these findings do not support the
practise of arthroscopic surgery for middle aged or
older patients with knee pain with or without signs
of osteoarthritis.
For more information
Arthroscopic surgery for degenerative knee:
systematic review and meta-analysis of benefits and
harms
2015;350:h2747
Arthroscopic surgery for degenerative knee
2015;350:h2983
MDN |